Undergraduate studies
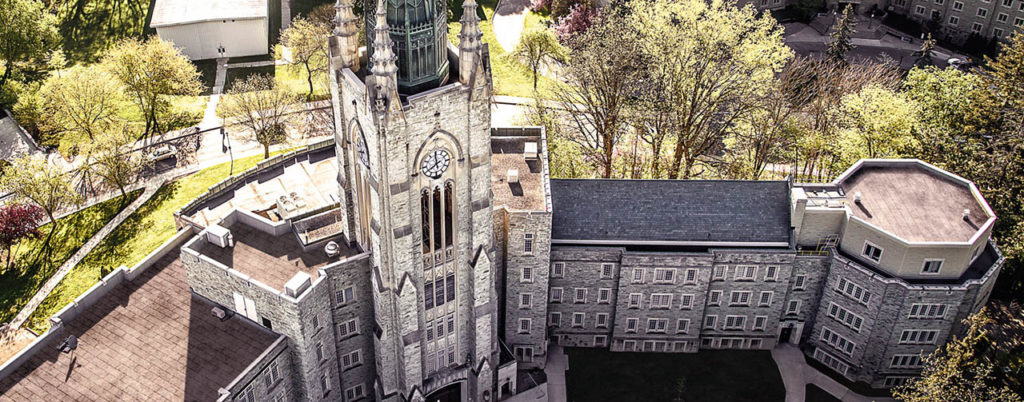
University of Western Ontario (UWO) also known as Western University in Canada, has a fantastic clinical neurological sciences department. In 2019, the Neuroscience at the UWO turned 50, and throughout these five decades, they have educated some brilliant minds. Studying at the University of Western Ontario’s clinical sciences department will help you acquire outstanding knowledge and skills, as well as witness the latest events in the neuroscience world.
In 2020-2021 due to the prolonged covid19 pandemic, the population’s involvement in online games and particularly in gambling, has increased in Canada. Since people work in self-isolation, they have more time for entertainment. As a result, the increased gaming activity drives the popularity of neuroscientific research on a gambler’s brain. Here are the most extensive ones in which our graduates participated:
- National Center for Responsible Gambling (Gambling and the Brain: Why Neuroscience Research is Vital to Gambling Research)
- National Center for Biotechnology Information (Pathological Choice: The Neuroscience of Gambling and Gambling Addiction)
- Current Biology (Inactivation of Medial Frontal Cortex Changes Risk Preference).
The annual research funding exceeds $225 million, and the quality of the studies is top-notch. The undergraduate program in neurosciences provides students with the latest methods and approaches to research each year.
Graduate studies
When it comes to graduate studies, the Department of Neurosciences at Western University has a unique program for students who want to study neuroscience with an interdisciplinary approach. Graduating from this program provides graduate students with an MSc or Ph.D. title in Neuroscience. The opportunities don’t end here since UWO will help you find full-time neuroscience internships. Your studies during these periods will be much easier since UWO has constant contact with employers that are looking to hire new interns.
Postdoctoral Competitive Edge Program
It is an excellent opportunity for all the postdoctoral scholars at Western since it helps them strengthen their resume and prepare themselves better for the job market. The objective of this program is to assist postdoctoral scholars by providing them with mentorship opportunities such as hypothesis development, research design, grant writing, research team management, and job search preparation, among other things. This is a very effective and practical program. The Professional Development Plan (PDP) is a tool that is used to decide the long-term and short-term goals of every postdoctoral scholar in the Neuroscience field. It is a very beneficial tool that can help postdoctoral students maximize their success.
Opportunities at London Health Sciences Centre

The London Health Sciences Centre is a huge hospital network. It offers excellent opportunities for young Ph.D. scholars that are looking to apply their knowledge in a professional setting. This will be the best place to start climbing the career ladder in the neurology field. Explore different branches of this network to find the right one for you.
Opportunities at University Hospital in London, Ontario
University Hospital in London, Ontario is a part of that network and is considered a good place to start your career. It has a complete Neuroscience Unit, that is equipped with 63 beds, 8-bed epilepsy monitoring unit, and the acute stroke monitoring unit. The University Hospital is a very coveted place because it contains EEG and EMG labs, the Neuromuscular Clinic, the Multiple Sclerosis Clinic, and the Stroke Prevention Clinic.
These clinics offer:
- Diagnosis
- Neurological conditions treatment
- Stroke prevention and treatment
- Brain aneurysm treatment
- Neuromuscular and degenerative disorders treatment

The greatest advantage for those looking to start their career in the neuroscience field at the University Hospital is the experience they will get from working with some of the brightest minds and cutting-edge technology.
The Pediatric Neurology Program that is located within the Children’s Hospital offers care when it comes to children that have neurological conditions. Being part of a group that consists of highly educated and motivated pediatric neurologists provides a competitive but also cooperative work environment that is highly beneficial to fresh Ph.D. scholars.
Urgent Neurology Clinic in London, Ontario
As a new neurologist in London, Ontario, you may also want to consider the urgent neurology clinic, which is a part of the Victoria Hospital. The reason why many new neurologists covet this place is that it only deals with urgent cases and those are usually very sensitive. The experience that young neurologists can gain by working in this hospital is unique because of their employment of the latest methods to deal with different urgent neurological issues in patients. As opposed to the London Health Sciences Centre, the Urgent Neurology Clinic in London, Ontario deals with cases that require immediate attention. With the help that Ph.D. scholars will get from the Postdoctoral Competitive Edge Program the chances of getting employed at one of the places mentioned above are high.
